Episode 36- Do we have to correct hyperglycemia in the ER?
Episode Summary:
Is routine correction of hyperglycemia in the ER necessary? And if so, which agents and routes are recommended? Find out this week!
Show Notes:
Key Points:
“Do we have to correct hyperglycemia in the ER?”:
– In a retrospective review of 422 adult patients who had a glucose level of 400 mg/dL or greater (mean 491 mg/dL) during their ER stay, there was no association between discharge glucose levels and either repeat visit for hyperglycemia or hospitalization, or the development of DKA and HHS. Actually, 2% of patients developed hypoglycemia due to the interventions
– If the team wants to lower glucose levels prior to discharge, use the patient’s own sliding scale if they are on insulin at home or use your institution’s sliding scale for hospitalized patients to get an estimated dose
– Another option is to use nursing-driven tools validated in the ER setting, such as the the Rush Emergency Department Hyperglycemia Intervention (REDHI) protocol (see image below)
– When choosing which insulin to give, stick to rapid-acting insulins such as aspart and lispro, and stick to the SQ route. IV regular insulin should be reserved for diabetic emergencies (DKA/ HHS) or shifting of hyperkalemia. Regular insulin has a pharmacokinetic profile that is not ideal for ER patients (peak at 3 hours with a 6-8 hour duration) vs rapid-acting insulins (peak at 1 hour with a 3 hour duration)
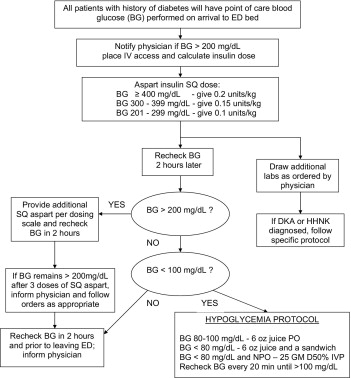
Rush Emergency Department Hyperglycemia Intervention (REDHI) protocol. This nurse-driven protocol attempted to lower the glucose level to a goal of < 180 mg/dL. After the nurse asked the patient when they last took their insulin or oral diabetes agents, they calculated a weight-based dose of SQ insulin based on the patient’s glucose level. They would then recheck glucose every 2 hours and continue to follow the protocol. By using this protocol, they were able to lower glucose by 175 mg/dL and lower the mean hospital LOS by 1.5 days compared to historical controls (P < 0.05); however, mean LOS in the ER was not affected. Keep in mind that this protocol came with a 7% risk of hypoglycemia.
References:
Transcript:
We’ve all seen the patient in the ER who happens to have elevated glucose levels. Now obviously if the patient is in a diabetic emergency such as DKA or HHS, we treat these patients with fluids and usually a continuous infusion of IV regular insulin.
We know that in the inpatient setting, glucose control (with goals usually around < 180 mg/dL) has been associated with better outcomes. But what about a patient who is in your ER with moderate hyperglycemia or a completely non-related concern whom you plan to discharge? Should we aggressively correct their glucose to a specific value? Does it have any bearing on their bounce-back rate?
Back in 2016, a study was published in the Annals of Emergency Medicine to answer this question. They did a retrospective review of adult patients who had a glucose level of 400 mg/dL or greater during their ER stay, and excluded patients who were admitted to the hospital or had type 1 diabetes. They ended up with 566 ER encounters in 422 patients, 58% were men and the mean age was 47 years. The mean arrival glucose level was 491 mg/dL. In 341 encounters, or 60% of cases, both IV fluids and SQ insulin was given to reduce glucose levels. Mean glucose reductions were 157 mg/dL and mean glucose values at discharge were 334 mg/dL (with a range of 48 – 694 mg/dL).
The authors looked at a 7-day follow-up period and found the following. Outcomes for return ER visits for hyperglycemia and hospitalization occurred in 13% and 7% of patients, respectively. DKA occurred in only 2 patients, and 0 patients developed HHS or died. All in all, there was no association between discharge glucose levels and either repeat visit for hyperglycemia or hospitalization, or the development of DKA and HHS. Actually, 2% of patients developed hypoglycemia due to the interventions. The authors concluded that “attaining a specific glucose level level before discharge in patients with hyperglycemia may be less important than traditionally thought.”
But what if your patient is being admitted, or if they have type I DM, which were exclusion criteria in the previous study? Or, what if you just really want to lower those levels prior to discharge or if you are still unsure about patient disposition?
Your go-to answer should be a rapid-acting, SQ insulin such as lispro (Humalog) or aspart (Novolog). To get to a dose of SQ insulin, if your patient is on insulin at home, just ask them how many units of insulin they would give themselves with that particular glucose value. If the patient is not on insulin at home, you have a couple of options. One option is to use your institutions sliding-scale insulin protocol to determine what the nurses on the floor would give your patient with that specific glucose value. Or, we can use some well-developed SQ insulin protocols that are specific to the ER setting, like the Rush Emergency Department Hyperglycemia Intervention (REDHI) protocol. And although this protocol attempted to lower the glucose level to a certain goal, of < 180 mg/dL in this case, and we just learned that this is probably unnecessary, its still worthwhile looking into this protocol. This is a nurse-driven protocol that would trigger if glucose levels were > 200 mg/dL. After the nurse asked the patient when they last took their insulin or oral diabetes agents, they calculated a weight-based dose of SQ insulin based on the patient’s glucose level. They would then recheck glucose every 2 hours and continue to follow the protocol. I’ll post this protocol to the errxpodcast Instagram page and to errxpodcast.com. By using this protocol, they were able to lower glucose by 175 mg/dL and lower the mean hospital LOS by 1.5 days compared to historical controls (P < 0.05); however, mean LOS in the ER was not affected. Keep in mind that this protocol came with a 7% risk of hypoglycemia.
Notice that I did not mention SQ or IV regular insulin as treatment options. At my institution, we try to avoid IV insulins outside of the setting of DKA/HHS or shifting of hyperkalemia. There really is no need to use IV insulin when we can use the SQ route. If you remember the pharmacokinetic data of insulins, regular insulins peak at about 3 hours and can have a 6-8 hour duration of action. Rapid-acting insulins peak within 1 hour with a duration of about 3 hours- which is a much better profile for the typical ER patient’s duration of stay. Not only can we cause hypoglycemia with IV insulins remember that giving IV insulin also lowers potassium levels; a recent study out of the ER setting found that patients given > 5 units IV regular insulin had an 8% risk of hypokalemia- which is just another small reason to not use the IV route routinely.
In conclusion, remember that for patients discharging from your ER, there is probably no need to normalize their hyperglycemia unless they are in a diabetic emergency. The most important intervention you can make is to make sure the patient has proper out-patient follow-up and adequate supplies of medications. If you still aren’t convinced, consider using SQ, rapid-acting insulins instead of IV or SQ regular insulin to try to lower those glucose levels. Using the patient’s own sliding-scale algorithm, using your institutions algorithm for hospitalized patients, or using ER-specific protocols such as the REDHI are good places to start.
As always, thank you so much for your time. Please remember to sing up for our newsletter on errxpodcast.com.
