Episode 84- “It Takes 1 to Roc”: Part One: ABW, IBW, or LBW?
Episode Summary:
In Part One of this “Mini Grand Rounds” series, we discuss the factors that determine how to dose meds, in this case rocuronium, in obesity
Show Notes:
Key Points:
“‘It Takes 1 to Roc’: Part One: ABW, IBW, or LBW?”:
– A drug’s volume of distribution (Vd) tells us the extent to which it distributes into body/fat tissue compared to the bloodstream/extracellular fluid. A higher Vd means more tissue distribution and a lower Vd means that drug stays mostly in the bloodstream/ extracellular fluid
– One of the most important factors affecting a drug’s Vd is its lipophilicity. A highly lipophilic drug leaves the bloodstream and distributes out to adipose tissue and therefore has a higher Vd. A non-lipophilic (ie. hydrophilic) drug mostly stays in the bloodstream and has a lower Vd
– If the Vd is low (~ 0.1-0.4 L/kg), the drug stays mostly in the bloodstream. If the Vd is moderate (0.6-5 L/kg), the drug is slightly lipophilic and distributes evenly throughout the blood and tissues. If the Vd is high (~ > 5 L/kg) the drug is very lipophilic and distributes out mostly into fat tissue. Most experts agree that we should use an Ideal Body Weight (IBW) or an Adjusted/Lean Body Weight when dosing drugs with a low Vd in obesity
– For hydrophilic, low Vd paralytics like rocuronium (Vd 0.25 L/kg) and vecuronium (Vd ~0.3 L/kg) use an IBW
– For moderately lipophilic drugs, like etomidate (Vd~ 3 L/kg), ketamine (Vd ~2.5 L/kg), propofol (Vd 2-10 L/kg), and midazolam (Vd 1-3 L/kg) use a Lean or an Adjusted Body Weight
– There are some exceptions. Succinylcholine, despite its low Vd, is dosed off of Actual Body Weight (ABW) or Adjusted/Lean Body Weight- not an IBW. This is because the enzyme that metabolizes it, plasma pseudocholinesterase, is present in higher levels in obese patients
– Alternatively, propofol (Vd 2-10 L/kg) and midazolam (1-3 L/kg) are lipophilic and should technically be dosed off of an ABW- but we don’t do that because at higher doses both of these agents can cause hypotension. In the setting of RSI, dose propofol and benzos off of their Adjusted/ Lean Body Weights, or even an IBW if you’re really worried about hypotension
– Many use a soft max dose of 100 mg for roc. Using a dose of 1 mg/kg IBW, almost all of your obese patients should do well with this dose- since you’d have to be ~ 7 feet tall to have an IBW of 100 kg
Please click HERE to leave a review of the podcast!
Transcript:
Hello and welcome to Episode 84 of ER-Rx, a podcast tailored to your clinical needs. I’m your host, Adis Keric. “It takes 1 to roc”- we’ve all heard the saying, an easy way to remember dosing rocuronium for RSI. It means that we should give 1 mg/kg. But what if you have an obese patient? Do you use their Actual Body Weight (ABW)? Or maybe you ignore all that extra fat tissue and just use an Ideal Body Weight (IBW)? Or how about using a dose somewhere in between those two and going with an Adjusted or Lean Body Weight (LBW)? In Part One of this “Mini Grand Rounds” series, I’ll be talking about which body weight to use when dosing roc in the obese patient. That’ll branch out into how to dose the rest of our RSI meds in obesity as well. Next time in Part Two of the series, I’ll talk about which mg/kg dose of roc may be the most effective for first-pass success- and it may not be the 1 mg/kg we all thought it was.
Rapid sequence intubation (RSI) involves giving induction agents followed by paralytics to optimize intubation conditions. The two most commonly used paralytics are succinylcholine and roc. Historically, at least at my site, succinylcholine was the heavy favorite, but in the last few years it seems like the use of roc has been increasing. So much so that at my site, I’d guess that over 90% of intubations in the ER are done using roc- which was the complete opposite when I first started practicing- and no, that wasn’t really that long ago. If you remember from a recent Instagram poll I sent out- most of my listeners also prefer roc to succinylcholine. But how do you dose roc in an obese patient? I personally recommend roc be dosed off of an IBW in obesity given its low volume of distribution (Vd). So, let’s go back to Pharmacology 101 for a couple of seconds and review what a drug’s Vd means.
In rough terms, it tells us the extent to which a drug is distributed into body or fat tissue compared to the bloodstream and extracellular fluid, with a higher Vd meaning a greater amount of tissue distribution and a lower Vd meaning that drug stays mostly in the bloodstream and extracellular fluid. One of the most important factors affecting a drug’s Vd is its lipophilicity. If it’s a highly lipophilic drug, that means it leaves the bloodstream and distributes out to tissue, typically adipose or fat tissue. If the drug is not lipophilic (in other words it’s hydrophilic) it means the drug tends to stay in the bloodstream. So, a highly lipophilic drug has a higher Vd, and a drug that is not lipophilic usually has a lower Vd. If the Vd is low, around let’s say 0.1-0.4 L/kg, it means the drug tends to hang around in the bloodstream and doesn’t distribute into out fat tissue. If the Vd is moderate, somewhere around 0.6- 5 L/kg, it means the drug is slightly lipophilic and distributes evenly throughout the blood and tissues. If the Vd is high, like anything greater than ~5 L/kg and sometimes even exceeding 100 L/kg, it means that the drug is very lipophilic and distributes out mostly into fat tissue.
Although dosing of meds in obesity is controversial and complex, most experts agree that we should use an IBW or an Adjusted/Lean Body Weight when dosing drugs with a low Vd. This brings us back to roc, with its Vd of only 0.25 L/kg. This means that you don’t have to take into account an obese patient’s entire body weight and all of that extra fat tissue because the drug just won’t go there. Roc will tend to stay in the bloodstream, so it makes sense to dose it off of an IBW that largely ignores all that extra fat tissue.
So how can you work this into your practice? Try to keep this in mind: For hydrophilic, low Vd paralytics like rocuronium (Vd 0.25 L/kg) and vecuronium (Vd ~0.3 L/kg) use an IBW.
For moderately lipophilic drugs, which happen to be all of your induction agents, like etomidate (Vd~ 3 L/kg), ketamine (Vd ~2.5 L/kg), propofol (Vd 2-10 L/kg), and midazolam (Vd 1-3 L/kg) use a Lean or an Adjusted Body Weight—which will be somewhere between a patient’s ABW and IBW.
Now let’s talk about some outliers. Succinylcholine, despite its low Vd, is actually recommended to be dosed off of an ABW or Adjusted/Lean Body Weight- not an IBW. This is because the enzyme that metabolizes it, plasma pseudocholinesterase, is present in higher levels in obese patients.
On the flip side, propofol (Vd 2-10 L/kg) and midazolam (1-3 L/kg) are pretty lipophilic and should technically be dosed off of an ABW- but we don’t do that because at higher doses both of these agents can cause hypotension, especially in an unstable patient who needs to be intubated. At higher doses these agents also tend to stick around much longer. That’s why in this setting, we should be dosing propofol and benzos off of their Adjusted/ Lean Body Weights, or even an IBW if you’re really worried about hypotension.
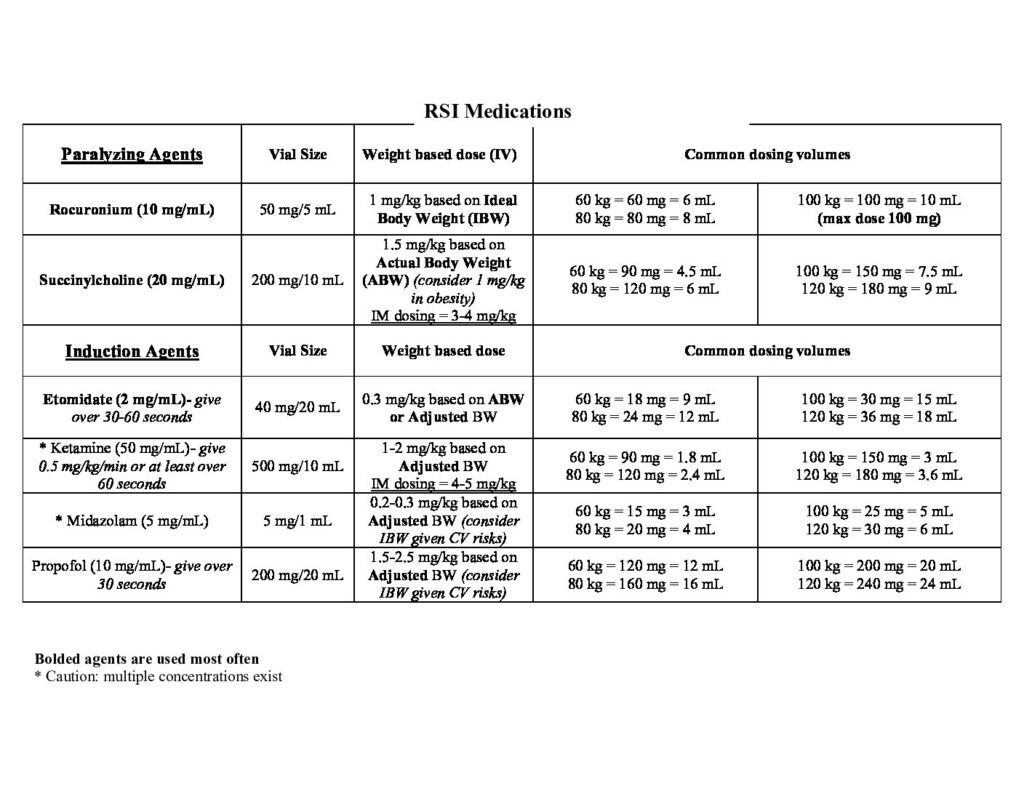
I know that all of this can be very hard to remember in an intense RSI situation. I’ll post a table of RSI meds and their dosing weights onto errxpodcast.com and the @ERRxPodcast Instagram page for you to reference. Another thing you can do is just use an Adjusted or Lean Body Weight for all of your RSI meds in obese patients since that’s just much easier to remember. Calculators for determining a patient’s Ideal, Adjusted, and Lean Body Weights can be found on free apps like MDCalc and Calculate by QxMD.
To wrap up- be very mindful when dosing RSI meds in the setting of obesity. Obese patients may weigh twice as much as an average patient, but that doesn’t mean they have twice the blood volume. For drugs with low Vd and low lipophilicity that tend to stay in the bloodstream, dosing off of an IBW makes clinical sense and has proven to be safe and effective. This is especially the case if you’re intubating with roc. Dosing an obese patient based on their ABW can greatly increase the duration of roc—even doubling it. This is one reason why I personally use a soft max dose of 100 mg for roc. Using a dose of 1 mg/kg IBW, almost all of your obese patients should do well with this maximum dose- since you’d have to be about 7 feet tall to have an IBW of 100 kg. That being said, next time, we’ll discuss how to best dose roc—in obese and non-obese patients. So, until the next episode, let’s change the saying to “it takes 1 (based on IBW) to roc.”
As always, thank you so much for your time, and thank you for wanting to learn more about pharmacotherapy. If you have any comments or anything you’d like to add to this episode, please give me a shout out on the @errxpodcast Instagram page, or reach out to me on errxpodcast.com- I’d love to respond to all comments and criticisms.
I also want to take a second to shout out friend-of-the pod and one of our stellar past pharmacy residents, Matt, for his very generous donation on BuyMeACoffee.com- donations like his help keep the podcast running and free for everyone. If you’d like to sponsor an episode, the link to donate is super easy to get to. It’s linked in the bottom of the episode description wherever you get your podcasts, on YouTube, and on the website. I’ll see you next time in Part Two of this series
References:
