Episode 51- How do we manage pain in patients on Suboxone?
Episode Summary:
In this episode, we discuss how to manage acute and post-op pain in patients on opioid maintenance therapy with Suboxone.
Show Notes:
Key Points:
“How do we manage pain in patients on Suboxone?”:
– Buprenorphine (Bup) is a high-affinity partial agonist at the mu opioid receptor with a long half-life (24-60 hours) and slow dissociation from the mu opioid receptor
– Historically, it’s been thought that the partial agonist activity of bup interferes with the analgesic activity of full opioid agonists. This has led to providers holding bup for patients in acute pain or prior to surgical intervention- which we now know isn’t the best course of action
– Bup has additive effects when used in combination with opioid agonists at their respective analgesic dose ranges. For bup, this dose range is around 8-12 mg sublingually. Only higher doses of bup outside of this general range lead to antagonistic analgesic effects
– In terms of opioid receptor availability, about 50-70% of mu opioid receptors are available with a 2 mg bup dose, 30-50% at a 4 mg dose, 10-20% at doses between 8 -16 mg, 5-15% at 24 mg doses, and only about 2-10% at 32 mg doses. At moderate doses (8-12 mg) there is still up to 20% mu-opioid receptor availability. This dose range corresponds well to bup’s analgesic dose
– If there are enough receptors available, we can add on additional mu-opioid agonists for additive analgesic effect
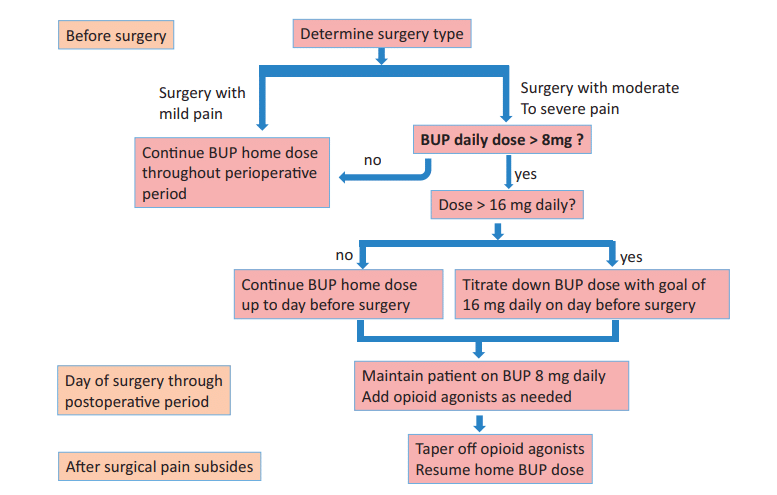
– One site developed an algorithm for management of surgical patients on bup (see image below). If the surgery was anticipated to result in only mild pain, or if patients were taking doses < 8 mg/day, then patients continued this dose peri-operatively and anticipated the need for higher opioid doses as needed
– If the surgery was expected to result in moderate to severe pain, bup doses were adjusted. If patients were on doses between 8-16 mg/day, they continue their home dose up to the day prior to surgery, and then on the day of surgery through the post-op period they were maintained on 8 mg/day
– If patients were on > 16 mg/day, they were titrated down to a goal dose of 16 mg on the day prior to surgery, then maintained on 8 mg/day on the day of surgery through the post-op period
– Remember that at the dose of 8 mg/day we are still in bup’s analgesic dose range, while still having at least 20% of our mu-opioid receptors available for pure opioid agonists to work on. At the same time, the 8 mg dose occupies more than 50-60% of the mu-opioid receptors which is required to prevent withdrawal
Source: Perioperative Management of Buprenorphine: Solving the Conundrum. Pain Medicine. 2019
One site’s recommendations for managing post-operative pain in patients on chronic buprenorphine therapy. If the surgery was anticipated to result in only mild pain or if patients were taking doses < 8 mg/day, then patients continued this dose peri-operatively and anticipated the need for higher opioid doses as needed. If the surgery was expected to result in moderate to severe pain, bup doses were adjusted. If patients were on doses between 8-16 mg/day, they continue their home dose up to the day prior to surgery, and then on the day of surgery through the post-op period they were maintained on 8 mg/day. If patients were on > 16 mg/day, they were titrated down to a goal dose of 16 mg on the day prior to surgery, then maintained on 8 mg/day on the day of surgery through the post-op period.
Please click HERE to leave a review of the podcast!
Transcript:
Hello and welcome to Episode 51 of ER-Rx. This week, we discuss how to manage acute or post-operative pain in patients on chronic buprenorphine therapy.
More than 2 million Americans have opioid use disorder (OUD), with over 100 deaths attributed directly to opioid-related overdoses every day. Opioid maintenance therapy has been proven to reduce opioid-related hospitalizations and mortality. On the flip side, evidence shows that patients have up to a 90% relapse rate if they are non-compliant with opioid maintenance therapy.
One agent that we use for opioid maintenance therapy is buprenorphine. Bup is a high-affinity partial agonist at the mu opioid receptor and is primarily a full antagonist at the kappa opioid receptor. Bup is associated with less opioid-induced hyperalgesia, causes less euphoria, and has a ceiling effect for respiratory depression. Bup has a long half-life of 24-60 hours when administered sublingually, and it also has very slow dissociation from the mu opioid receptor- meaning that it has a relatively long duration of action. Given this, regular full opioid agonists (like our classic opioids) and antagonists (like naloxone) can’t easily kick bup off once it binds to mu opioid receptors. Bup typically comes in the combination product Suboxone- which includes naloxone. Remember that the naloxone component doesn’t get absorbed orally or sublingually and is only in the product to prevent it from being crushed and injected IV.
It’s been widely thought that the partial agonist activity of bup interferes with the analgesic activity of full opioid agonists. But we often forget that bup is still an opioid and does have analgesic activity. As a matter of fact, we have preclinical and clinical trials showing that bup has additive effects when used in combination with opioid agonists at their respective analgesic dose ranges. For bup, this dose range is around 8-12 mg sublingually. Only higher doses of bup outside of this general range lead to antagonistic analgesic effects. This tells us that we may have to modify the home bup regimen or use higher doses of pure opioid agonists in patients with acute or post-op pain.
Another thing to consider is opioid receptor availability. In vivo studies, we show that about 50-70% of mu opioid receptors are still available with a 2 mg bup dose, 30-50% at a 4 mg dose, 10-20% at doses between 8 -16 mg, 5-15% at 24 mg doses, and only about 2-10% at 32 mg doses. Overall, these studies suggest that high bup maintenance doses (24-32 mg) leave barely any open mu-opioid receptors, whereas at moderate doses (8-12 mg) there is still up to 20% mu-opioid receptor availability. Interestingly this dose range corresponds well to bup’s analgesic dose mentioned previously.
If there are enough receptors available with bup in the system, we can still add on additional mu-opioid agonists for analgesic effect. We also know that about 50-60% receptor occupancy is required for bup to have adequate opioid withdrawal symptom suppression- meaning most patients will need a dose of at least 4 mg to prevent withdrawal.
How do we put all of this together? Historically, experts recommended discontinuing bup 3-5 days prior to surgery and supplementing with opioid agonists to reduce withdrawal. More recently, others have recommended continuing bup throughout the pre and post-surgical periods. There is still some controversy as to which option is best, but in general both populations- those that held bup and those that continued it- had similar reductions in pain scores and other patient-specific outcomes, although they each required higher opioid doses than the general population- but some of this can be explained by opioid tolerance or opioid- induced hyperalgesia. Given that the risk of opioid abuse increases when bup is discontinued, most experts now recommend simply continuing bup peri-operatively- sometimes at lower doses.
One site developed an algorithm for management of surgical patients on bup. I’ll post an image of this algorithm onto errxpodcast.com and the @errxpodcast Instagram page. If the surgery was anticipated to result in only mild pain, or if patients were taking doses < 8 mg/day, then they simply continued this dose perioperatively and anticipated the need for higher opioid doses as needed.
If the surgery was expected to result in moderate to severe pain, bup doses were adjusted. If they were on doses between 8-16 mg/day, they were told to continue their home dose up to the day prior to surgery, and then on the day of surgery through the post-op period they were maintained on 8 mg/day.
If they were on > 16 mg/day, they were titrated down to a goal dose of 16 mg on the day prior to surgery, then maintained on 8 mg/day on the day of surgery through the post-op period. Remember that at the dose of 8 mg/day we are still in bup’s analgesic dose range, while still having at least 20% of our mu-opioid receptors available for pure opioid agonists to work on. At the same time, the 8 mg dose occupies more than 50-60% of the mu-opioid receptors which is required to prevent withdrawal.
In each case patients were given opioid agonists on an as needed basis. Remember that you’ll need to use opioids that have high intrinsic activity at the mu-opioid receptor; things like morphine, fentanyl, and hydromorphone- for best effects. It’s also very important in these scenarios to use multimodal analgesia with NSAIDs, gabapentin, and possibly ketamine to reduce opioid exposure. Once surgical pain subsides, all patients were tapered off opioid agonists and resumed their home bup doses.
Of course, there are different ways of managing this patient population. Some sites continue the patient’s home bup dose without any reductions- knowing they’ll need much higher opioid doses to achieve pain control. Some continue the home dose but divide it into 3-4 times/ day dosing to take advantage of bup’s 6-8-hour analgesic activity. Some temporarily increase the home bup dose up to 32 mgs per day and divide that into 3-4 daily doses. And lastly, some recommend continuing bup at home dosing and only reducing the dose if adjunct therapies and opioid agonists fail to control pain. All of these are viable options; it’s only becoming clearer that the least effective option is discontinuing bup therapy altogether.
And as a side note- for patients on methadone for opioid maintenance therapy we again simply continue their home methadone dose and maximize non-opioid analgesics while allowing for PRN opioids at higher doses.
In conclusion, in patients on chronic opioid maintenance therapy with bup who are in acute or post-op pain, stopping bup in hopes of achieving better pain control may not be the best course of action. Usually continuing or slightly adjusting their bup dosing with higher doses of as needed opioids is the best option. Consider involving your hospital’s addiction or pain medicine experts when managing these patients, as well as having long discussions with your patients about their wishes and reasonable expectations.
As always, thank you so much for your time. We are nearing the 52nd episode of ER-Rx and our one-year anniversary. To celebrate, we’ll be doing another small prize giveaway. To enter, simply leave a review of the podcast on Apple Podcasts, then send me a message on errxpodcast.com with your review and email address.
References:

I have cervical stenosis and three pinched nerves two going in different directions without full use of my hands and arms I’m going to need surgery. I am currently on Suboxone and am it does nothing for my pain and even tried increasing the dose to see if it did. What doctor should I see in terms of switching to an opiate to control my pain before surgery
I had a dental abscess and my doctor would not treat my pain or call my Subutex doctor for advice. I suffered for 2 weeks until it but with continuous hot compress. When it burst my mouth was full of blood and pus. No wonder I was in agony.
If I was a regular patient they would have rushed me into the office and treated the abscess and given me Percocet
I’m so sorry to hear that– there definitely are strategies we can use to treat acute pain, like you were having, even if you are on Suboxone/ Subutex.
There needs to be help for us on subutex who are severely injured our doctors leave us to suffer Suboxone or subutex does not work for Dental pain or chronic pain we are turned down and told by doctors are hands are tied which is only gonna cause seeking to relive our severe pain I tired of being looked at as a pos or less of a person
Charles,
I completely understand your frustration. We definitely need to educate more on how to manage pain in patients taking Suboxone.