Episode 33- Shock through the heart: Is two better than one?
Episode Summary:
What is dual/double defibrillation? How does it work? Does it improve outcomes? Find out this week!
Show Notes:
Key Points:
“Shock through the heart: Is two better than one?”:
– Refractory ventricular fibrillation (RVF) is defined as VF that persists after 3 defibrillation attempts. Last line options for patients in RVF include esmolol (see Episode 21) and/or dual defibrillation (DD)
– DD uses 2 defibrillators and 4 pads on the patient while shocking. Pads can be placed in the “anterior-anterior” or “anterior-posterior” positions (see image below)
– Shocks can be delivered “simultaneously” or “sequentially.” There is no difference in efficacy between the different pad placement or shock delivery options
– A recent meta-analysis including 4 studies showed that DD was not superior to standard defibrillation, with similar rates of sustained ROSC (28.1 % vs 36.4%), survival to admission (30.7% vs 36.9%), and survival to discharge (10.2% vs 14.5%). There were no adverse events reported when using DD
– Remember that the results are still inconclusive due to the low quality of evidence of the trials included in the meta-analysis, which only included patients with out-of-hospital cardiac arrest
– Overall, the authors recommend that DD can still be attempted as a potential life-saving option, but there is not enough evidence to consider this a standard of care. The 2020 AHA guidelines recommend against the use of DD
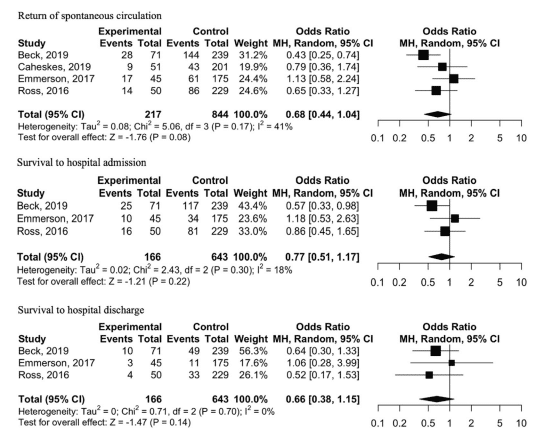
Forest plot of comparison for adults treated with dual defibrillation as compared to standard defibrillation for refractory ventricular fibrillation in the setting of out-of-hospital cardiac arrest. Squares or diamonds to the right of the solid vertical line favor dual defibrillation, but this is only significant (p <0.05) if the horizontal lines do not cross the solid vertical line.
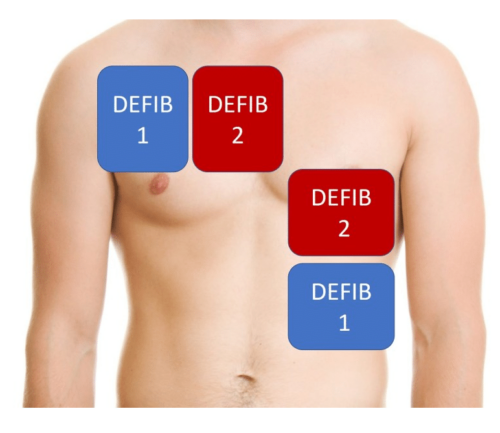
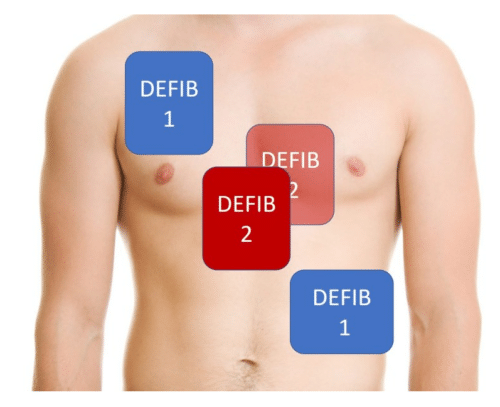
The image on the left shows the “anterior-anterior” pad placement option. The image on the right shows the “anterior-posterior” pad placement option, with the second defibrillator pad on the patient’s back.
Sources: Double defibrillation for refractory in-and-out-of-hospital cardiac arrest: a systematic review and meta-analysis. J Emerg Med. 2020; 59 (4): 531-541
References:
Transcript:
Hello and welcome to Episode 33 of ER-Rx. This week, we discuss a meta-analysis published in the Journal of Emergency Medicine that reviewed dual defibrillation in cardiac arrest.
Refractory ventricular fibrillation (RVF) is defined as persistent VF with no response to three or more defibrillation attempts. Its estimated that about 10-25% of cardiac arrests can develop RVF, with a mortality rate of up to 97% if this occurs. Since there is no proven treatment for this entity, people have looked at doing things like giving esmolol (and we talked about this in Episode 21) and other things such as dual/double defibrillation.
Dual defibrillation is just what it sounds like- using 2 defibrillators and 4 pads on the patient while shocking. When doing this, the team will grab an identical defibrillator, and then the team has the option of 2 different pad placements, which is of course in addition to the 2 pads that the patient already has on. The first option (“anterior-anterior”) is placing the pads right next to the first set, and the second option (“anterior-posterior”) places one pad between the other two pads, and the second pad on the patient’s back. I’ll post an image of this on the errxpodcast Instagram page and errxpodcast.com. It’s very important here that the pads don’t touch so that we don’t destroy the defibrillators.
Dual defibrillation comes in two flavors: simultaneous and sequential. If you want “dual simultaneous defibrillation,” it’s best to have one provider push the “shock” button at the same time. However, if you want to attempt “dual sequential defibrillation,” then it may be best to have two different providers push “shock” on each defibrillator to try to get a more sequential effect. Remember that there is no difference in efficacy between the two pad placement options or shock sequence options.
Dual defibrillation has shown some success in terminating RVF in a few case reports and observational studies. But how does it work? Some say that using 2 defibrillators instead of one will, obviously, deliver more energy, hopefully making defibrillation more effective. Another theory is that the first shock, even if delivered milliseconds before the second shock, can lower the defibrillation threshold, which then improves the second shock’s success. Lastly, another theory is that the more pads you place on the patient, the more vectors our electrical shock has to reach a greater number of myocytes.
This particular systematic review and meta-analysis was published to see if dual defibrillation had any effect on in- and out-of-hospital cardiac arrests. This trial ended up including only 4 studies in its meta-analysis due to a lack of high-powered trials on dual defibrillation overall. And we have to remember, the studies included were from out –of-hospital cardiac arrests, as the authors couldn’t find any eligible trials that looked at in-hospital cardiac arrests. The four studies included in the meta-analysis had 1,061 patients, with 217 receiving dual defibrillation and the rest receiving standard defibrillations. All were retrospective cohorts studies. Most patients received dual defibrillation after 3 failed standard defibrillations, the patients were mostly male (76 – 92% depending on the study) and the mean age was 59-62 years in both groups. Around 60% in each group were witnessed arrests and about 50% receiving bystander CPR. They found similar rates of sustained ROSC (28.1 % vs 36.4%), survival to admission (30.7% vs 36.9%), and survival to discharge (10.2% vs 14.5%). There was no statistical significance either at the individual study level (except for improved rates of ROSC in one study) or in the overall the meta-analysis level, showing no evidence that dual defibrillation is better than standard single defibrillation. The good news was that there was no significant adverse events reported. The authors concluded that although dual defibrillation had no effect on any outcomes of interest, the results are still overall inconclusive due to the lack of firm evidence, and they call for further investigation. This is because the quality of evidence of the 4 trials included in the meta-analysis was very low, and none of them were randomized controlled trials. Also, keep in mind that this was a cohort of out-of-hospital cardiac arrest patients, who have worse outcomes than patients who arrest in the hospital. Overall, the authors recommend that dual defibrillation can still be attempted as a potential life-saving option, but there just isn’t enough evidence to consider this a “standard of care.”
What do the guidelines say? Although anxiously-awaited, I feel like the recent cardiac arrest guidelines released in October 2020 didn’t really add too much. However, this guideline recommends against the use of dual defibrillation, citing systematic reviews finding no evidence that dual defibrillation is effective. I guess we’ll have to wait until the “DOSEVF” trial comes out. This is a randomized, crossover trial in, hopefully, over 900 patients, that will attempt to answer the question of whether or not dual defibrillation is useful. But we can’t expect results until 2022.
In conclusion, although kind of promising in case reports and retrospective studies, dual defibrillation should not be routinely used. To be fair, if the team wanted to attempt this, there hasn’t been much evidence of patient harm. Also, while you’re at it, you may as well try a bolus of 500 mcg/kg of esmolol prior to the dual shocks to help optimize outcomes.
As always, thank you so much for your time, and see you next week.
