Episode 23- The ammonia level: what is it good for?
Episode Summary:
Should we be using ammonia levels to diagnose, determine the severity, or monitor the resolution of hepatic encephalopathy?
Show Notes:
Key Points:
“The ammonia level: what is it good for?”:
– Hepatic encephalopathy (HE) is a result of excess nitrogenous substances, such as ammonia, that cause changes in neurotransmission
– Lactulose is considered first-line therapy for lowering the production and absorption of ammonia. When lactulose is metabolized by gut microflora, it creates an acidic environment which kills the ammonia-producing bacteria and inhibits the diffusion of ammonia into the systemic circulation
– Despite lactulose’s ammonia-lowering effects, there is almost no correlation between ammonia levels and mental status
– In one study, when using ammonia levels of > 55 micromol/L to diagnose HE, the positive predictive value was 77% and the negative predictive value was 48%. Patients with normal ammonia levels can have HE, and those with elevated ammonia levels do not necessarily have HE
– Studies have shown that patients can clinically improve with the same or even increasing ammonia levels, or can continue to have symptoms while levels decrease
– In conclusion, HE should be a clinical diagnosis independent of ammonia levels, and serial ammonia levels should not guide treatment
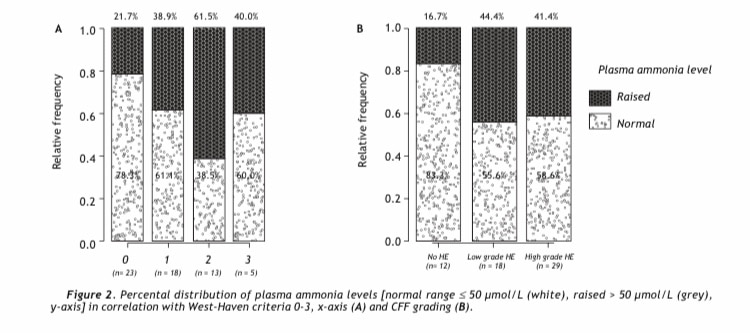
Plasma ammonia levels can be normal (white bars) even if patients have West-Haven criteria Grade 1-3 hepatic encephalopathy, and they can be elevated (grey bars) even in patients who have no hepatic encephalopathy
Source: How to diagnose hepatic encephalopathy in the emergency department. Ann Hepatol. 2013; 12 (1): 108-114
References:
Transcript:
Hello and welcome to Episode 23 of ER-Rx. This week, we talk about something that you may commonly see in your ER, or during hospital and ICU rounds: the checking of ammonia levels for patients with liver disease or for those with hepatic encephalopathy (HE). Are ammonia levels diagnostic? Can we use these levels to monitor for HE resolution?
HE is a CNS disturbance that is associated with hepatic insufficiency and liver failure—up to 70% of patients with cirrhosis may suffer from HE. HE happens when nitrogenous substances, such as ammonia, enter the systemic circulation and are unable to be detoxified by the damaged liver. These substances then cause changes in neurotransmission that affect consciousness and behavior.
First-line treatment of HE is, as usual, non-pharmacologic, and the first goal is to identify and treat precipitating factors (mainly infection and GI bleeds), which may be enough to reverse the encephalopathy. Pharmacologic therapies may also be added, and they include mainly therapies that lower ammonia. Lactulose, a non-absorbable disaccharide, is considered first-line for lowering the production and absorption of ammonia. Lactulose is metabolized by the gut microflora into acetic and lactic acid, producing an acidic environment in the gut which kills the ammonia-producing bacteria. As a bonus, when lactulose is metabolized, it inhibits the diffusion of ammonia into the systemic circulation.
We know through multiple studies that lactulose works for treating HE, whether alone or in combination with things such as polyethylene glycol or rifaximin. However, although lactulose is thought to mainly work by reducing ammonia levels, there is almost no correlation between ammonia levels and mental status. One reason may be due to the fact that ammonia levels may be falsely low or high for any given blood draw. For example, things such as high-protein meals, hypokalemia, and certain drugs such as diuretics and valproic acid can increase ammonia levels. Even simple things like using a tourniquet or clenching the fist during blood draws can increase ammonia levels. Even if we have perfect collection methods, studies have shown poor correlation between ammonia levels and diagnosing or monitoring of HE resolution.
For example, one study from an ER setting showed a positive predictive value of only 77% and a negative predictive value of 48% when using ammonia levels of > 55 micromol/L to diagnose HE. Also, 60% of patients with Grade 3 HE had a normal ammonia level. I’ll post an image from that study onto the errxpodcast website and Instagram page. Suffice it to say, ammonia levels may be a decent rule-in test (in combination with clinical signs/symptoms), but a poor rule-out test. All in all, this and other studies have shown that patients with normal ammonia levels can have HE, and those with elevated ammonia levels do not necessarily have HE.
So we probably shouldn’t use ammonia levels alone to diagnose HE, but how about to monitor for its resolution? If we serially collect levels and they go down, this is must be a good thing, right? What if they go up again- do we need more lactulose? The answer again is “no”. Studies have shown that patients can clinically improve with the same or even higher ammonia levels, or can continue to have symptoms while levels decrease.
In conclusion, HE should be a clinical diagnosis independent of ammonia levels. The degree of elevation of the ammonia level does not correlate well with the severity of HE, and serial ammonia levels have limited usefulness in monitoring therapy– remember that ammonia levels are not even included in HE staging. So, although we routinely use therapies that work by lowering ammonia levels, obviously, there are other substances at play here.
Another thing to mention is that lactulose dose and frequency should be titrated to your goal stool output and serial clinical exams, not necessarily the ammonia level—your nurses may thank you for this.
As always, thank you for your time. We recently hit a big milestone this week with over 5,000 downloads. We continue to accept feedback and recommendations for future episodes- it is your feedback that led to recent episodes on toxicology and pre-hospital cardiac arrest. Feel free to reach out to us on errxpodcast.com, or on our Instagram page: “errxpodcast.”
