Episode 45- How do we treat agitation in the ER setting?
Episode Summary:
This week, we discuss which agents to use to control agitation in a few different clinical scenarios encountered in the ER.
Show Notes:
Key Points:
“How do we treat agitation in the ER setting?” :
– Overall, start with oral agents and prioritize second-generation, atypical antipsychotics over first-generation antipsychotics. Wait 10 minutes before repeating a dose if the med was given IV, 20 minutes if it was given IM, or 2 hours if it was given PO
– In the setting of delirium, first find and fix the underlying cause. If the delirium is due to alcohol or benzodiazepine withdrawal, use PO/IV/IM benzodiazepines and avoid haloperidol and droperidol
– If the delirium is not due to alcohol or benzodiazepine withdrawal, use PO risperidone, olanzapine, or haloperidol. If we can’t give oral agents, use IM or IV olanzapine, droperidol, or haloperidol. Avoid benzodiazepines in this setting as they can worsen delirium
– In the setting of intoxication with a CNS stimulant, use PO/IV/IM benzodiazepines. In intoxications due to a CNS depressant, avoid benzodiazepines and instead use first-generation antipsychotic agents such as PO/IV/IM haloperidol or IM/IV droperidol. Second-generation antipsychotics don’t have a lot of data in this setting
– In the setting of psychosis, prioritize PO risperidone, olanzapine, or haloperidol +/- benzodiazepines. In this setting, we oftentimes include a benzodiazepine with the antipsychotic. IM/IV agents include droperidol or haloperidol +/- benzodiazepines
– Ketamine is used for patients with profound agitation who are actively violent and are an immediate danger to themselves or to staff. We typically use 250 mg IM (or 4 mg/kg), repeated x 1 after 5 minutes to a total dose of 500 mg. If we have IV access, we use a dose of 50-100 mg every 2 minutes until adequate sedation is reached
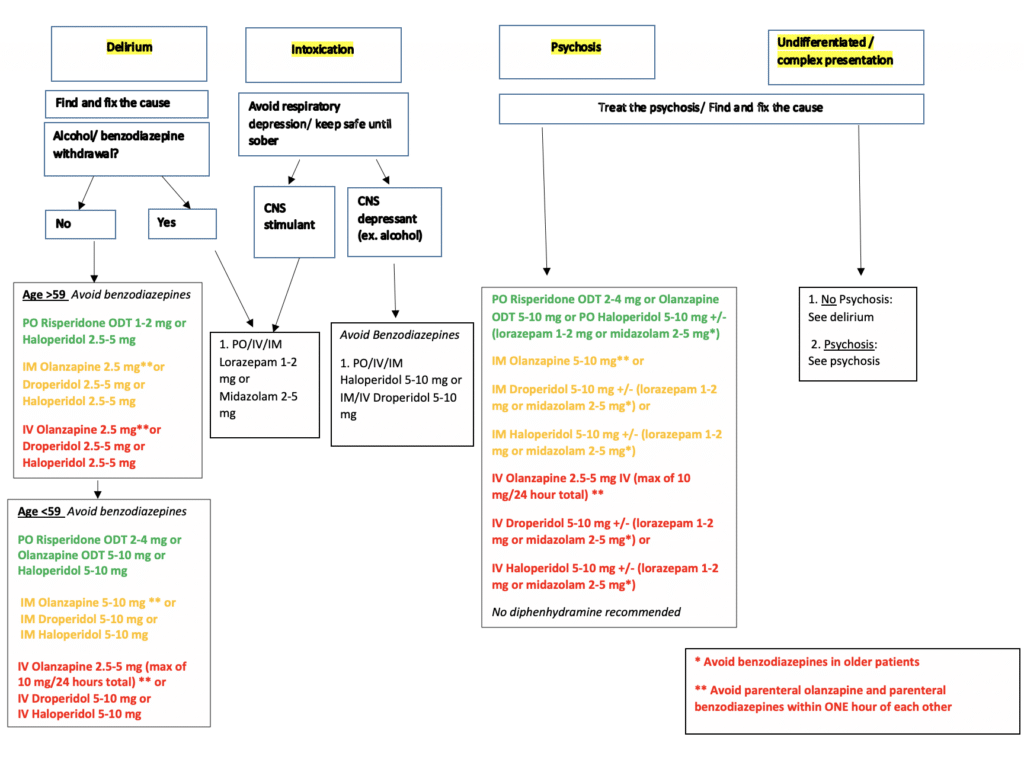
This is one example of an ER-specific agitation treatment protocol. As discussed in the episode, prioritizing oral agents (when possible) and second-generation/ atypical antipsychotics is recommended. Doses listed are general guidelines that must be adjusted to each individual patient. This guideline is largely repurposed from the American Association for Emergency Psychiatry Project BETA workgroup, and is referenced below in the Read by QxMD collection for this episode.
Please click HERE to leave a review of the podcast!
Transcript:
Hello and welcome to Episode 45 of ER-Rx. This week, we review some of the medications that we use to control agitation in the ER setting. Overall, at my site we follow the guidance from the American Association for Emergency Psychiatry- Project BETA workgroup.
The first thing that we consider when treating agitation is; what is the cause of the agitation? A few of the main causes we consider are delirium, intoxication, and psychosis.
If the agitation is thought to be due to delirium, the definitive treatment is finding and fixing the underlying cause. Often removing the trigger will at least help reduce some of the agitation, and if not, we have medications that can help. As an overall rule, we typically start with oral agents, if the patient is willing and able to take them, and we prioritize using second-generation, atypical antipsychotics over first-generation antipsychotics given their better side effect profile. You’ll notice that throughout this episode. Also, as a refresher, make sure you check out Episode 9 for my take on droperidol’s use for agitation, and why it’s one of my favorite agents to use in the ER setting. Lastly, to get a sense of the doses we use, please check out the agitation protocol posted on the ER-Rx podcast Instagram page and on errxpodcast.com.
Ok, getting into the meds. If the delirium is due to alcohol or benzodiazepine withdrawal, we give PO/IV/IM lorazepam (1-2 mg) or midazolam (2-5 mg) and we try to avoid haloperidol and droperidol. Easy.
If the delirium is not due to alcohol or benzodiazepine withdrawal, we have several options. In elderly patients (aged > 60) we start with PO risperidone (1-2 mg) or haloperidol (2.5 -5 mg). Risperidone is a great second-generation antipsychotic that has some of the best safety and efficacy data in this setting, and it also has a shorter time to peak than other oral agents. If we can’t give oral agents, use IM or IV olanzapine (2.5 mg), droperidol (2.5-5 mg), or haloperidol (2.5-5 mg). We use lower dosing in elderly patients and we avoid benzodiazepines, which can actually worsen agitation and delirium in this setting and in this patient population.
Similarly, in younger patients (aged < 59), we again prioritize oral routes and second-generation antipsychotics but at slightly higher doses. (For PO agents we try risperidone 2-4 mg, olanzapine 5-10 mg, or haloperidol 5-10 mg. IM/IV dosing for droperidol and haloperidol is 5-10 mg. For olanzapine, we use 5-10 mg IM or 2.5-5 mg IV (with a maximum of 10 mg /24 hours if given IV)). Again, try to avoid benzodiazepines even in younger patients who are delirious.
Next, if the agitation is due to intoxication, we first decide if the intoxicant was a CNS stimulant or a CNS depressant. If it was a stimulant (such as meth), we use PO/IV/IM lorazepam or midazolam. If it was a CNS depressant (like alcohol), we avoid benzodiazepines. As an exception to one of our general rules, we use first-generation antipsychotic agents such as PO/IV/IM haloperidol (5-10 mg) or IM/IV droperidol (5-10 mg), with droperidol showing slightly better efficacy than haloperidol in this setting. Second-generation antipsychotics don’t have a lot of data in the setting of agitation due to CNS depressants- so we typically don’t use those as much.
In the setting of psychosis, the agents we use are very similar to those used in the setting of delirium. Once again, we prioritize PO risperidone, olanzapine, or haloperidol +/- lorazepam or midazolam. In this setting, we often-times include a benzodiazepine with the antipsychotic, given these combinations have been shown to work faster and may even have less side effects than giving the antipsychotic alone. IM/IV agents include droperidol or haloperidol +/- lorazepam or midazolam.
When using IV or IM olanzapine, we avoid parenteral benzodiazepines within one hour of the olanzapine as per package insert recommendations. I know that this is a controversial topic, with some studies showing that parenteral olanzapine and benzodiazepine agents can be used together- but I just won’t get into this for the sake of time. Also, notice that we try to not use diphenhydramine or B52 combinations at my site. We also don’t use much ziprasidone given its inferiority compared to other agents and its significant QTc prolonging effects.
Of course, you will adjust your combinations and doses in clinical practice, with older, smaller patients requiring smaller doses, and younger, bigger, more agitated patients requiring higher doses. We also give higher doses to patients who are chronically on high doses of neuroleptic agents at home. We usually wait 10 minutes before we repeat a dose if the med was given IV, 20 minutes if it was given IM, or 2 hours if it was given PO– but remember that this is after the maximum dose is given. For example, if you give 5 mg haloperidol IM, and the patient is still very agitated at 5-15 minutes, you can repeat the 5 mg dose safely.
Lastly, we do also have the option of using ketamine as well. I’ll be honest, ketamine isn’t my favorite agent for agitation, and I’ve seen it lead to even more agitation, delirium, and aggression- especially in patients who have substance abuse histories or those with psychiatric issues. That being said, I do believe there is a place in therapy for ketamine. At my site, ketamine is used for patients with profound agitation who are actively violent and are an immediate danger to themselves or to staff. These patients may also be suffering from excited delirium- especially in the setting of known sympathomimetic drug abuse. In this setting, we give 250 mg IM (or 4 mg/kg) into a large muscle, repeated x1 after 5 minutes to a total dose of 500 mg. If we have IV access, we use a dose of 50-100 mg every 2 minutes until adequate sedation is reached. Keep in mind that these patients need critical care level of monitoring, as they may require intubation.
In conclusion, fixing the underlying cause of the agitation and verbal de-escalation always come before giving medications. Also, determining the cause of the agitation is key to choosing the most appropriate agent for your specific patient.
As always, thank you so much for your time. If you have any questions, comments, or anything to add to my discussion for this episode please leave a comment on errxpodcast.com or the ER-Rx Podcast Instagram page. Also remember that this show is available on Apple Podcasts, Google Podcasts, Pandora, Spotify, iHeartRadio, and even YouTube.
References:
