Episode 49- Annie are you A-OK?
Episode Summary:
This week, we talk about amniotic fluid embolism (AFE) and the “A-OK” medication combination.
Show Notes:
Key Points:
“Annie are you A-OK?”:
– Amniotic fluid embolism (AFE) is a complication of pregnancy where amniotic fluid enters the maternal pulmonary circulation causing sudden cardiovascular collapse. AFE is the second leading cause of maternal death in the US and Europe
– Signs/ symptoms of AFE include respiratory distress, cardiovascular collapse, and coagulopathy. Other symptoms include hypotension, loss of consciousness, hemorrhage, and seizure-like activity. Less commonly, disseminated intravascular coagulation (DIC) may be the initial presenting feature
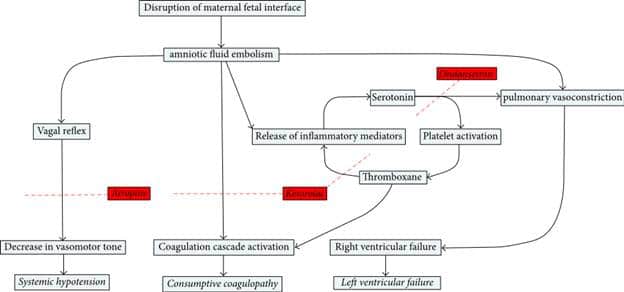
– The pathophysiology of AFE is unknown, but is thought to be a complex phenomenon involving numerous mediators that cause anaphylactoid reactions and complement activation once amniotic fluid enters maternal circulation. AFE may be in part caused by serotonin and thromboxane induced platelet dysfunction, degranulation, and pulmonary hypertension. Activation of factor VII and platelets also activates the coagulation cascade, causing DIC and eventually multi-organ failure
– Treatment is focused on early recognition and resuscitation. Priorities include controlling hemorrhage and reversing coagulopathy with TXA and massive transfusion protocols, hemodynamic support with fluids and vasopressors, respiratory support, and delivery of the fetus
– Based on anecdotal evidence and case reports, a combination of atropine, ondansetron, and ketorolac may be used for refractory cases. This “A-OK” regimen is directed at some of the mediators thought to cause or contribute to AFE
– Atropine (at a dose of 1 mg) blocks vagal stimulation and reverses parasympathetic activity that causes pulmonary artery spasm and vasoconstriction. It also reverses bradycardia that can occur during AFE
– Ondansetron (at a dose of 8 mg) blocks serotonin receptors, which are found in vagal terminals of the heart and lungs and cause pulmonary vasoconstriction
– Ketorolac (at a dose of 30 mg) blocks thromboxane, which is a major platelet activator
Source: Atypical Amniotic Fluid Embolism Managed with a Novel Therapeutic Regimen. Case Reports in Obs and Gyn. 2017
The proposed mechanism of the “A-OK” protocol in the setting of amniotic fluid embolism (AFE). Atropine (1 mg) blocks the vagal reflex and subsequent hypotension that occurs during AFE. It also reverses pulmonary artery spasm and vasoconstriction as well as bradycardia. Ondansetron (8 mg) blocks serotonin receptors, reversing pulmonary vasoconstriction and platelet activation. Ketorolac (30 mg) blocks thromboxane, halting the activation of the coagulation cascade and the release of inflammatory mediators.
Please click HERE to leave a review of the podcast!
Transcript:
Hello and welcome to Episode 49 of ER-Rx. This week, we’ll discuss amniotic fluid embolism (AFE) and a potential drug combination that can be used in this emergent situation. AFE is a complication of pregnancy where amniotic fluid enters the maternal pulmonary circulation causing sudden and catastrophic cardiovascular collapse. This is thought to occur from a combination of damage from the amniotic fluid debris and subsequent immune reactions. The true incidence of AFE is unknown, but estimates suggest that it happens in one in every 15,000 to 50,000 births. AFE is the second leading cause of maternal death in the US and Europe, with estimates suggesting a case fatality rate of 13-26%.
AFE is a clinical diagnosis made by exclusion. Typically, most patients develop respiratory distress, cardiovascular collapse, and coagulopathy. Other symptoms include hypotension, loss of consciousness, hemorrhage, and seizure-like activity. Some patients do present atypically with only respiratory failure and/or hypotension. Less commonly, disseminated intravascular coagulation (DIC) may be the initial presenting feature.
The Society of Maternal-Fetal Medicine and the Amniotic Fluid Embolism Foundation proposed a diagnostic definition of AFE research standardization which may also be used clinically. Per their definition, AFE is diagnosed with all 4 of: a sudden onset of cardiorespiratory arrest or hypotension with evidence of respiratory compromise, documentation of DIC, clinical onset during labor or within 30 minutes of delivery, and absence of fever during labor.
The pathophysiology of AFE is largely unknown, but is thought to be a complex phenomenon involving numerous mediators that cause anaphylactoid reactions and complement activation once amniotic fluid enters maternal circulation. Amniotic fluid is known to contain vasoactive and procoagulant products such as cytokines and thromboxane. Many believe AFE is in part caused by serotonin and thromboxane induced platelet dysfunction, degranulation, and pulmonary hypertension. Pulmonary hypertension begins with serotonin stimulation of serotonin receptors, which causes pulmonary vasoconstriction. Platelets become entrapped due to the vasoconstriction, and they then activate thromboxane. Thromboxane in turn causes recruitment of even more platelets, worsening pulmonary hypertension, which releases even more serotonin– completing an ongoing cycle. It’s thought that these mediators also cause vagal stimulation which leads to hypotension. Activation of factor VII and platelets also activates the coagulation cascade, causing DIC and eventually multi-organ failure.
Treatment is focused on early recognition and resuscitation. Remember that in the event of cardiac arrest, you’ll still continue with standard ACLS measures. Other priorities include controlling hemorrhage and reversing coagulopathy with TXA and massive transfusion protocols, hemodynamic support with fluids and vasopressors, respiratory support, and delivery of the fetus.
But we also have an interesting drug combination we can try. Based on anecdotal evidence and case reports, a combination of atropine, ondansetron, and ketorolac may be used for refractory cases. This “A-OK” regimen is directed at some of the mediators thought to cause or contribute to AFE.
Atropine (at a dose of 1 mg) blocks vagal stimulation and reverses parasympathetic activity that causes pulmonary artery spasm and vasoconstriction. It also reverses bradycardia that can occur during AFE.
Ondansetron (at a dose of 8 mg) blocks the serotonin receptors, which are found in vagal terminals of the heart and lungs and as mentioned cause pulmonary vasoconstriction.
Ketorolac (at a dose of 30 mg) blocks thromboxane, which is a major platelet activator.
I’ll post an image of the proposed mechanism of these drugs on errxpodcast.com and on the @errxpodcast Instagram page. I’ve personally never had to give the “A-OK” protocol, but it is something that we can consider in these cases. These medications are relatively safe and cheap and should be available in nearby automated medication dispensing machines, especially on OB units.
As always, thank you so much for your time. Please check out our website: errxpodcast.com. There, you can subscribe to our newsletter, which when we get enough subscribers, we’ll start sending out key points from previous episodes and other monthly tidbits.
References:
