Episode 14- SARS-CoV-2 antibody test
Episode Summary:
What does a negative or positive antibody test mean? Should it change our behavior? Do we have to view the results in the setting of where we are located? Tune in this week!
Show Notes:
Key Points:
“SARS-CoV-2 antibody test”:
– After infection with SARS-CoV-2, our immune systems develop IgG and IgM antibodies to the virus
– How long these antibodies remain and if they prevent future episodes of COVID is unknown at this time
– For now, these antibody tests help us determine which populations have been affected and therefore may have higher rates of herd immunity
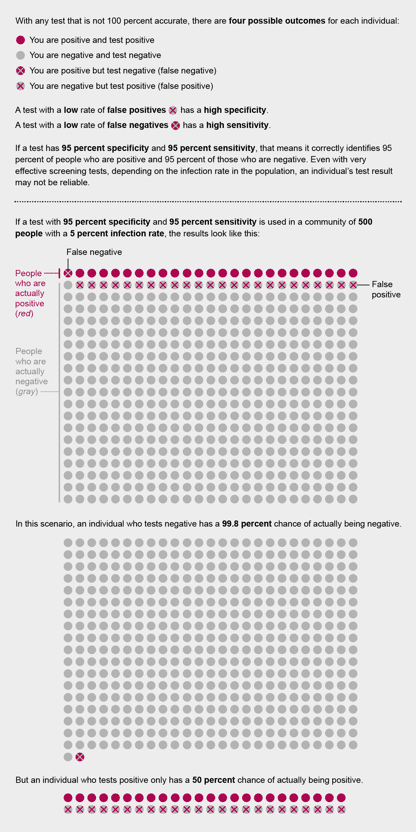
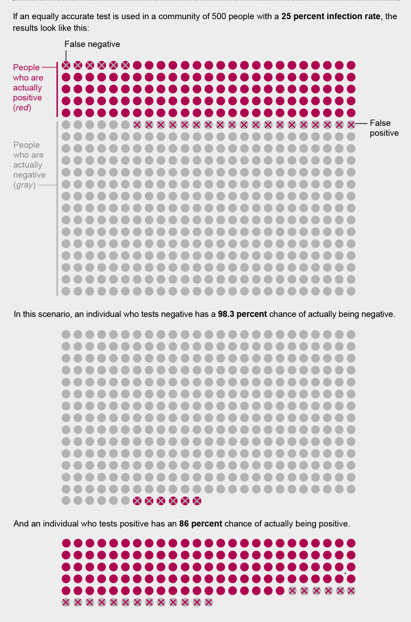
– A high “specificity” means that the test has a low rate of false positives, and a high “sensitivity” means that the test has a low rate of false negatives
– These are related to negative predictive value (NPV) and positive predictive value (PPV). If the test has high NPV, a “negative” test means you likely do not have the antibodies. If the test has high PPV, a “positive” test means that you likely do have the antibodies
– NPV and PPV are related to the prevalence of the antibodies in a population. The fewer people who have the antibodies in a population, the more likely it is that an individual’s “positive” result is wrong
– However, a “negative” test in a low prevalence population has a very high NPV. This is the situation where most of us will find ourselves in
– For example, if your antibody test has a 99.9% specificity and 100% sensitivity, and we assume most communities have a low prevalence (<5% -25%), a “negative” results is almost always a true result, but a positive test may just be a false positive
Credit: Amanda Montanez/ Scientific American Magazine
References:
Interim guidelines for COVID-19 antibody testing. CDC. May 23, 2020. Accessed July 7, 2020.
Abbott ARCHITECT SARS-CoV-2 IgG Instructions for Use. H14806R01. April 2020
Bryan A, Pepper G, Wener MH, et al. Performance characteristics of the Abbott Architect SARS-CoV-2 IgG assay and seroprevalence testing in Idaho. J Clin Microbiol. 2020; 00941-20
Frasier SL. Coronavirus antibody tests have a mathematical pitfall. Scientific American. 2020; 323(1): 12-13
Transcript:
Hello and welcome to Episode 14 of ER-Rx. Well, we finally got to this point. I’m doing my first COVID-related episode, and instead of rehashing the almost hourly barrage of information on treatments, morbidity, and mortality, I wanted to focus on something you can hopefully find useful for yourself and your patients. This week, we discuss the SARS-CoV-2 IgG antibody test and what its results mean in different settings. I recently got my antibody results and it came back negative.
Serologic assays for SARS-CoV-2 help determine whether or not the individual being tested was ever infected, even if they never had any symptoms. These tests do this by measuring the host’s immune response to the virus. Almost all people with functioning immune systems will develop some sort of immune response following SARS-CoV-2 infection. This means that our bodies will produce IgM and IgG antibodies within weeks of illness onset. The strange thing about SARS-CoV-2 is that IgM and IgG antibodies are formed almost at the same time in the serum, which is not the case for most infections, where IgG lags behind IgM. However, how long these antibodies remain detectable is not known.
Recurrence of COVID-19 appears to be uncommon, possibly due to the development of these antibodies. However, we do not have definitive data on this at this time, and these tests should not be used to determine absolute immunity from future infections. What these tests do is help determine how much of a population has been infected. This demographic and geographic information can help us understand which communities may have higher infection rates and therefore higher rates of herd immunity. They may also be used to determine who may qualify to donate blood used to manufacture convalescent plasma as a possible treatment option for those who are critically ill from COVID-19.
To better understand these types of tests, we have to talk a little bit about stats. The utility of these tests depends on sensitivity and specificity of the assays, which is related to the positive predictive value and the negative predictive value. As a quick review, “sensitivity” refers to the ability of a test to detect something if it is truly there. In this case, antibodies to SARS-CoV-2. Is it “sensitive” enough to turn positive if antibodies are present? This means that the higher the sensitivity, the lower rate we have of false negatives, meaning that if you have a negative test, it probably truly means you don’t have the antibodies.
“Specificity” refers to the ability of a test to only detect one certain thing, in this case only antibodies to SARS-CoV-2, but not other antibodies. This means that the higher the specificity, the lower rates we have of false positives, meaning that if you have a positive test, it truly means that you have the antibodies. These relate to positive and negative predictive values in this way: if the test has a high positive predictive value, it means that if you have a positive test, you almost certainly have the antibodies. If the test has a high negative predictive value, it means that if you have a negative test, you almost certainly do not have the antibodies. To throw a wrench in this, these values are determined by the percentage of antibody-positive individuals in the tested population, otherwise known as the “prevalence” of the disease.
For example, in a high-prevalence setting, the positive predictive value increases. However, in a low-prevalence setting, the positive predictive value drops because there are now more false-positive results. Said another way, the fewer people who have the antibodies in a population, the more likely it is that an individual’s positive result is wrong. And in contrast, the negative predictive value is higher in a low prevalence setting, and lower in a high-prevalence setting. I hope all of that wasn’t too confusing.
Suffice it to say that we really need to understand not only our facilities’ antibody test, but also the prevalence in our community. As far as the test goes, the one we at my site has 99.9% specificity and 100% sensitivity for detecting the IgG antibody. This comes with the caveat that the individuals are tested 17 days after symptom onset. To note, the earlier we test post-symptom onset, the worse the test does as there has not been enough time for these antibodies to form.
In terms of prevalence, in most of the country, including even the heavy hit areas, the prevalence of the antibody is thought to be low at <5% - 25%, so testing at this point likely means more false positive results and fewer false-negative results. I live in Minnesota and as a very rough estimate from the Minnesota Department of Health, we have at this point tested over 600,000 people and over 37,000 of those have had a positive PCR. This is approximately a 5% prevalence but once again, this is only a very rough estimate. So, in my case, my negative test had a very high negative predictive value and was likely accurate.
Does this change my behavior at work or in life? Not really. Would a positive result have changed my behavior? Once again not really because we don’t know what it means to have these antibodies at this time. I will basically go about my life and continue doing things I already have been doing: social distancing, wearing a mask, and keeping my hands clean and out of my face.
As always, thank you so much for your time. I will post a great article and a fantastic visual from Scientific American magazine that also describes what I went over in this episode onto errxpodcast.com and the @errxpodcast Instagram page.
