Episode 11- Anaphylaxis: A pharmacologic management update
Episode Summary:
What is the most important agent for anaphylaxis? What other treatments are only considered as adjuncts? How should I give these agents? Find out this week as we review updated anaphylaxis treatment guidelines published in April 2020!
Show Notes:
Key Points:
“Anaphylaxis: A pharmacologic management update”:
– Epinephrine (Epi) is the most important medication in the setting of anaphylaxis
– Epi reverses almost all of the signs/symptoms of anaphylaxis by vasoconstricting, bronchodilating, reducing mucosal edema, increasing cardiac output, and stabilizing mast cells and basophils
– The dose of Epi is 0.01 mg/kg intramuscularly (IM) with a max dose of 0.3 mg in children and 0.5 mg in adults. For children weighing 15- <30 kg, the Epi-Pen Jr auto-injector delivers 0.15 mg of Epi. Children >/= 30 kg and adults receive the full-dose Epi-Pen which delivers 0.3 mg of Epi. This can be repeated every 5-15 minutes
– If there is no response to 2-3 IM doses of Epi, we can start an intravenous (IV) infusion of Epi at 0.1 mcg/kg/min (or 2-10 mcg/min) and titrate to response
– Antihistamines (both H1 and H2) are given as adjunctive therapy only and are not meant to replace Epi. Diphenhydramine 50 mg IV (H1) and famotidine 20 mg IV (H2) are commonly used
– Corticosteroids are not routinely recommended in this setting but if used, consider methylprednisolone 125 mg IV x 1
– Biphasic anaphylaxis can occur up to 72 hours after the initial episode. Patients at risk of biphasic anaphylaxis who may require longer observation periods (up to 6 hours) include those who present with severe anaphylaxis and/or those who receive > 1 dose of IM Epi
– Antihistamines and glucocorticoids have not been shown to reduce rates of biphasic anaphylaxis
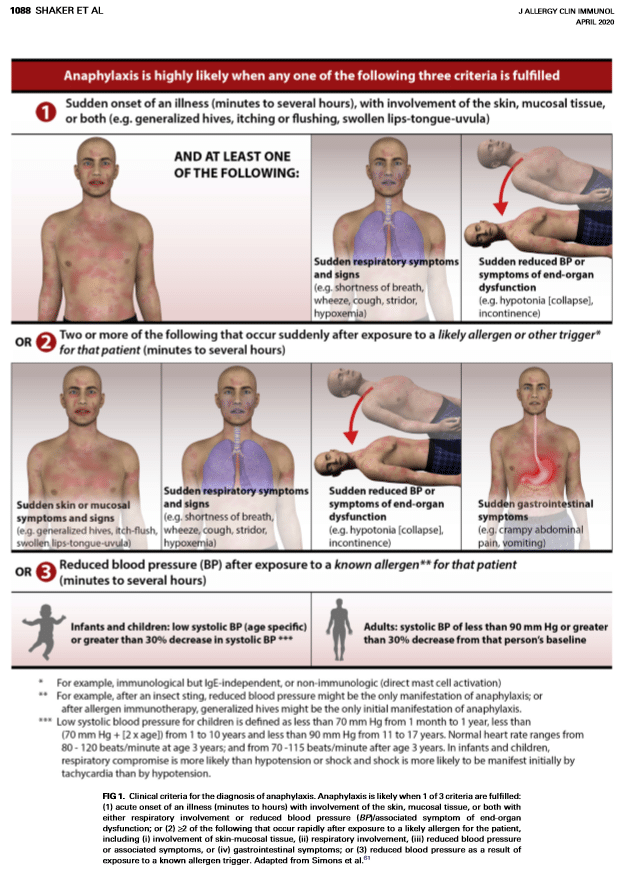
Clinical criteria for the diagnosis of anaphylaxis
References:
Transcript:
Hello and welcome back to ER-Rx. In this episode, we focus on the pharmacologic treatments of anaphylaxis in adults. After this episode you should be comfortable with knowing which is the most important agent, what doses should we use, and what are some practical implications providers, pharmacists, and nurses working in the ER should remember when treating a patient with an anaphylactic reaction.
Anaphylaxis is an acute life-threatening allergic reaction that may present with a wide range of manifestations. The diagnostic criteria mainly focuses on the abrupt development of skin and mucosal tissue symptoms in addition to respiratory and/or cardiovascular symptoms. I will post Figure 1 from these guidelines onto errxpodcast.com if you would like a more detailed diagnostic reference. In adults, medications (specifically antibiotics, NSAIDS, immunomodulators, and biological agents) as well as insect bites are the leading triggers of anaphylaxis, and in children the most common triggers are once again medications and also foods. Adverse drug reactions affect up to 10% of the population and up to 20% of hospitalized patients. This is a big deal and also why we as pharmacists spend so much time trying to get patients off unnecessary medications. The leading mechanism of anaphylaxis is IgE binding and cross-linking onto the surface of mast cells and basophils, but it can also involve neutrophils, monocytes, macrophages, and platelets as well as numerous complement components. Treatment consists of medications that affect most of these mechanisms and reduce the clinical symptoms of hives, itching, bronchospasm, and hypotension.
Most importantly, we have epinephrine. This magical drug treats all of the symptoms of anaphylaxis mentioned. As a nonselective agonist of all adrenergic receptors, epinephrine works rapidly to vasoconstrict, increase cardiac output, bronchodilate, reverse mucosal edema, and to stabilize those pesky mast cells and basophils. Although epinephrine is the most important aspect of anaphylaxis management, it continues to be underutilized. Thankfully mortality from anaphylaxis continues to be a very rare outcome at 0.3%, however, delayed use of epinephrine is associated with increased risk of mortality.
Epinephrine is administered intramuscularly into the outer thigh in a dose of 0.01 mg/kg using a 1:1000 (or 1 mg/mL) solution, with a maximum dose of 0.5 mg in adults and 0.3 mg in children. In patients weighing < 15 kg, the 0.01 mg/kg dose is prepared by using the 1 mg/1mL vial and drawing up the dose in a 1 mL syringe. If this will delay therapy, and if your site has auto-injectors, it is reasonable to give the Epi-Pen Jr (0.15 mg epinephrine) product for this weight. In patients weighing 15- <30 kg we will use the Epi Pen Jr., and anyone weighing >/= 30 kg gets the Epi Pen (0.3 mg epinephrine). These doses can be repeated every 5-15 minutes. National and international guidelines recommend giving epinephrine as an intramuscular injection rather than a subcutaneous injection based on pharmacodynamic studies that have shown a higher peak plasma concentrations and faster onset for the intramuscular route compared to the subcutaneous route. In patients without an adequate response after 2-3 doses of intramuscular epinephrine, we can start an intravenous infusion at 0.1 mcg/kg/min (or 2-10 mcg/min depending on how your site orders vasopressors) titrating to response. If you are concerned about the time it takes for an epinephrine infusion to come from IV pharmacy, consider setting up a protocol in your ER where the pharmacist can compound a standard-concentration epinephrine infusion at the bedside to expedite preparation times.
We also have a couple of second-line or adjunctive therapies. Antihistamines are considered second-line agents given their slow onset of action and their inability to stabilize mast cells or to target other causes of anaphylaxis. They also do not treat the cardiovascular and respiratory symptoms of anaphylaxis. However, they can be used to treat hives and itching to improve patient comfort. They should not be used in place of epinephrine and should not delay epinephrine administration. Of the 4 histamine receptors in the body, the H1 subtype is the most clinically relevant during anaphylaxis. H2 receptors are found mostly in the GI tract with minimal distribution in the vascular smooth muscle cells and play only a minor role in anaphylaxis. Nevertheless, H1 and H2 antihistamines are routinely given concurrently with epinephrine without much supporting data for their efficacy. We give 50 mg IV diphenhydramine (Benadryl). For H2 blockers we give famotidine (Pepcid), at a dose of 20 mg IV. If the anaphylaxis is not as severe and we are not worried about aspiration or decreased systemic absorption, these agents can be given orally, and if so, preferentially use second-generation H1 blockers such as loratadine can be given due to their longer duration of action and lower side effect profile.
Glucocorticoids are also used as an adjunct despite the poor evidence supporting any clinical benefit. Like antihistamines, glucocorticoids should not be used in place of epinephrine and should not delay epinephrine administration. Remember that glucocorticoids work by binding to the glucocorticoid receptor on cell membranes, being translocated to the nucleus, and inhibiting gene expression and production of inflammatory mediators. This is a long process and therefore the onset of action of these agents is very slow (benefit takes 4-6 hours). There are studies that show that their use is associated with reduced lengths of stay but they do not prevent readmission. The authors emphasize that glucocorticoids have a very limited role in the setting of anaphylaxis, but they may be beneficial for patients with severe symptoms requiring hospitalization or for those with known underlying lung disease with bronchospasm that persists after other symptoms have been controlled. The dose here is slightly controversial, but we usually give 125 mg IV methylprednisolone as this is the dose these vials come in. Alternatively, guidelines and medical references recommend 1-2 mg/kg or 50-125 mg IV as a single dose.
The guidelines also discuss biphasic anaphylaxis. In this scenario, the anaphylaxis recurs up to 72 hours after resolution of the initial episode. Rates are anywhere from <1% to 20%. The severity of anaphylaxis and/or the administration of > 1 dose of epinephrine are the factors that should guide a patient’s risk for developing biphasic anaphylaxis. The authors suggest extended clinical observation for those patients. Although low-risk patients can be discharged after a 1-hour observation period, high risk patients may need up to 6 hours or longer, including hospital admission. The authors also suggest against administering glucocorticoids or antihistamines specifically as an intervention to prevent these biphasic reactions. These adjunct medications have not been shown to prevent biphasic anaphylaxis as was once widely assumed.
In conclusion, my own takeaways from these guidelines echo the Good Practice statements of the authors. This includes administering epinephrine as the first-line agent at the doses discussed, not delaying administration of epinephrine, observing the patient until symptoms have resolved, and patient education including education on Epi-Pen use. All staff in the ER should be very familiar with intramuscular and intravenous epinephrine weight-based dosing regimens for all patient weights. Antihistamines and glucocorticoids, although given routinely at most sites, have not been shown to affect major clinical outcomes and should never delay epinephrine administration.
As always, thank you so much for your time. Please remember to subscribe to our Podcast at “ER-Rx”. You can find us on Apple Podcasts, Google Podcasts, Spotify, and YouTube.
